

Across the U.S., skilled nursing facility (SNF) capacity is shrinking — and the consequences are already being felt across hospitals, post-acute providers, and care coordination teams. While licensed bed counts tell one story, a new study published January 12, 2026 reveals a more urgent reality: operational SNF capacity — beds that can actually be staffed and used — is declining at a much faster rate than previously understood.For healthcare organizations navigating tighter margins, staffing shortages, and growing pressure to reduce length of stay, this trend has significant implications for discharge planning, referral management, and patient outcomes.
Recent national data shows that the U.S. is losing skilled nursing capacity — not just through facility closures, but through unusable beds driven by staffing and financial constraints.
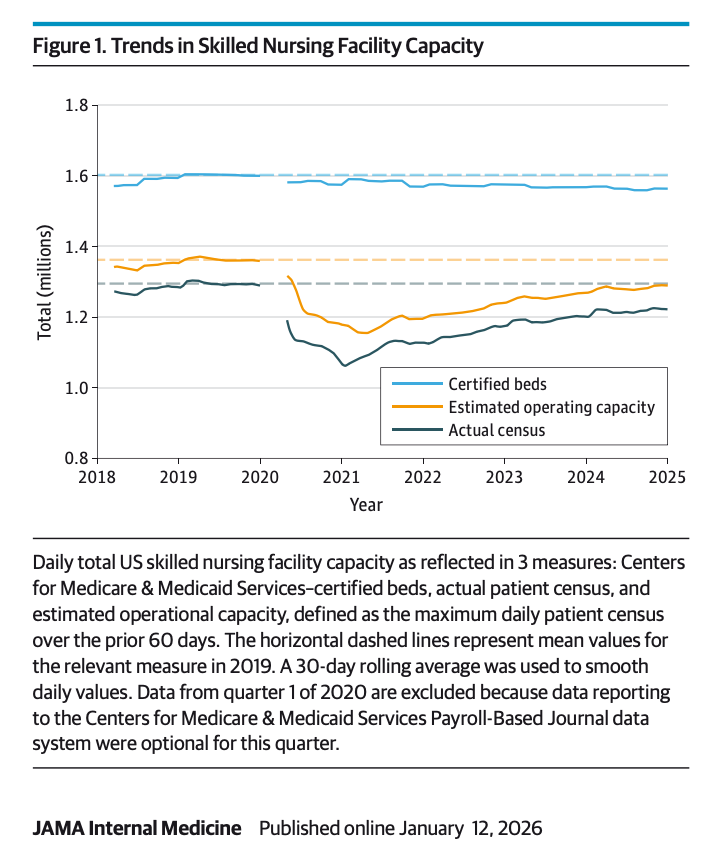
A JAMA Internal Medicine study published online January 12, 2026 found that while licensed SNF beds declined by approximately 2.5%, operating capacity fell by nearly 5% nationwide between 2019 and 2024. In more than a quarter of U.S. counties, operating capacity declined by 15% or more, with rural areas hit hardest.
Industry reporting reinforces this finding. Skilled Nursing News reports that many facilities technically remain open, but are forced to limit admissions or close units because they cannot staff them.
The result: fewer real options for hospitals trying to place patients who need skilled nursing care after discharge.
Staffing shortages — particularly among nurses and certified nursing assistants — remain the single biggest constraint on SNF operations. Even facilities with available physical beds are often unable to admit patients due to insufficient staffing coverage.
Rising labor costs, inflation, and reimbursement challenges — especially within Medicaid — are forcing many operators to reduce capacity or exit markets altogether. According to the American Health Care Association (AHCA), access to nursing home care is worsening as facilities struggle to stay financially viable.
More patients prefer home- and community-based services, which influences payer models and investment decisions — but demand for skilled nursing care has not disappeared. Instead, it has become harder to meet when capacity is constrained.
Ongoing discussions around federal staffing mandates and funding reforms add uncertainty for SNF operators, making long-term workforce and capacity planning more difficult.
The decline in skilled nursing capacity doesn’t stop at the post-acute level — it directly affects hospital operations and patient flow.
Research shows that areas with less SNF capacity experience:
Patients in regions with larger capacity declines see worse discharge outcomes and increased journey distances for placements.
As skilled nursing availability becomes more volatile, many healthcare organizations are increasingly turning to AI-driven insights to anticipate capacity constraints, identify discharge risk earlier, and support faster, more informed decision-making across care transitions.
As skilled nursing capacity tightens, healthcare organizations need better visibility, faster coordination, and more proactive planning. Cascala supports this shift by enabling smarter, data-driven care transitions across the continuum.
In an environment where SNF availability can change daily, coordination and insight are no longer optional.
Declining skilled nursing capacity is not a short-term disruption — it reflects deeper workforce, financial, and policy challenges reshaping post-acute care nationwide. As availability becomes less predictable, healthcare organizations need more than manual processes and static reports to keep care moving.
This is where AI-enabled intelligence becomes increasingly critical.
Cascala leverages AI to help organizations identify emerging capacity constraints, surface discharge risk earlier, and prioritize next-best actions across transitions of care. By transforming complex operational data into actionable insight, Cascala supports faster, more confident decision-making — even as skilled nursing capacity continues to decline.
Rather than reacting to bottlenecks after they occur, healthcare teams can use AI-driven insight to anticipate challenges, coordinate more effectively, and maintain continuity of care in a constrained post-acute environment.
Contact us to learn how Cascala supports smarter post-acute planning — or schedule a demo to see how Cascala combines AI-driven insight with integrated workflows to help healthcare organizations adapt to post-acute capacity constraints and keep care moving.